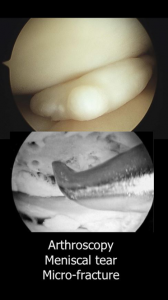
- Arthrocopy
- ACL Reconstruction
- Total Knee Replacement
- Partial Knee Replacement
- Patella Stablisation
- Revision of Knee Replacement
 Before the day of admission it is helpful for you to have read consent information about your procedure. This information can be downloaded here
Before the day of admission it is helpful for you to have read consent information about your procedure. This information can be downloaded here
As you are having an arthroscopy you will normally only be in hospital for the day. The nursing staff will provide you with a sick certificate prior to discharging you.
You will leave with a large bandage on your knee which will be removed a few days later at an appointment in the hospital with the nursing staff. It is really important that you continue to do the exercises you were shown in hospital once you get home.
You should take regular painkillers if needed - usually a combination of Ibuprofen and Paracetamol is sufficient. Simon will see you in the ward before you are discharged home. His practice manager will forward you a copy of your operation note and you will be given the operative photographs to keep.
In terms of driving, you should not drive for a week following arthroscopy unless it is your left knee and you have an automatic car which will allow you to drive after 48-hour is. You will be signed off work for 2 weeks.
Simon will see you again at the 2-week post-operative stage when he will check the wound and movement of the knee. If all is well you can return to work at this point. He will also take the opportunity to discuss the findings at the time of surgery.
 Before the day of admission it is helpful for you to have read consent information about your procedure and the rehabilitation protocol for ACL reconstruction which will be followed by your physiotherapist following the operation. This information can be downloaded here. You are usually only in hospital for a day with this procedure.
Before the day of admission it is helpful for you to have read consent information about your procedure and the rehabilitation protocol for ACL reconstruction which will be followed by your physiotherapist following the operation. This information can be downloaded here. You are usually only in hospital for a day with this procedure.
This procedure is carried out arthroscopically through a telescope which is inserted into your knee through a small cut (keyhole) although in addition you will also have an incision over the upper part of the lower leg which will allow harvest of the hamstring graft and insertion of the graft through the knee. Immediately following your operation an X-ray of your knee will be carried out to confirm the position of the devices used to hold the reconstruction in place. Clips are used to close the wound and these will be removed 2 weeks after your operation.
Prior to going home Simon will see you and discuss what was found at the time of the procedure. You will also be seen by the physiotherapists who decide whether you need crutches and they will show you the initial exercises you need to practice to maximise your recovery. Prior to your discharge you will be provided with an injection into the abdomen to reduce the risk of deep vein thrombosis and will be provided with anti-embolism (TED) stockings which you should wear for 2 weeks. Occasionally it will be necessary for you to be sent home with further injections to be continued. When you leave you will have a large bandage on your knee and an appointment will have been made for you to return to see the nursing staff after several days for this to be removed. The physiotherapists will also arrange for you to have a physiotherapy follow-up appointment at around a week following your surgery.
It is really important that you continue to do the exercises you were shown in hospital once you get home. You should take regular painkillers if needed - usually a combination of Ibuprofen and Paracetamol is sufficient.
You can return to driving once you feel confident which is approximately a week after your operation. It is really important that you follow the exercises provided in the rehabilitation protocol to ensure that you get a good outcome following your surgery. You should take at least 2 weeks off work. A certificate will be provided by the hospital prior to discharge if you need it. Simon will provide a further certificate when you come back to outpatients if there is any requirement for further time off.
Simon will see you again at the 2-week post-operative stage. He will discuss the findings of your surgery again and will also examine your knee to check the range of movement, the wound, clinically exclude deep vein thrombosis and test stability of the joint. The nursing staff will remove the clips from your wounds at that time. Provided all is well Simon will allow you to increase exercise aimed at strengthening the knee and maximising range of movement but will also recommend that you continue the physiotherapy follow-up.
Further physiotherapy continues up to approximately 3 months following your surgery and is usually on a weekly basis initially increasing to fortnightly when appropriate. Simon will continue to review your progress and you will be seen at the 2-month and 4-month post-operative stage by him. In terms of returning to sport, this will be guided by your overall knee strength and the time following your surgery. In some cases it will be possible to return to sport around 4 months following your surgery but in other cases this will need longer. It takes up to a year for your recovery following anterior cruciate ligament reconstruction to reach an endpoint.
During your recovery slight numbness over the front of the shin is common and initially it is common to experience marked bruising through the calf and into the foot. During recovery the knee often swells after exercise and this can take up to 6 months to resolve.
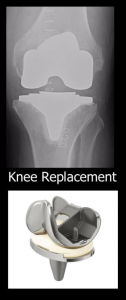 Before your admission it is helpful for you to read the consent and information about the type of knee replacement you are going to have which will be sent to you or can be downloaded here.
Before your admission it is helpful for you to read the consent and information about the type of knee replacement you are going to have which will be sent to you or can be downloaded here.
Simon’s preferred total knee replacement is the Attune knee replacement manufactured by DePuy. This knee replacement was launched in the United States in 2010 and the UK in 2012. As this knee replacement does not yet have a 10 year track record Simon follows the recommended guidelines of entering your information into “beyond compliance”. This requires you to sign a separate consent form to allow your data to be shared with the company who manufacture your knee replacement. This can be downloaded here.
More information about the outcome of the Attune knee replacement in general can be found here. The purpose of beyond compliance is to ensure an early warning system should there be any concerns about the longevity of this knee replacement.
In 2017 the 4-year outcome data from the National joint Registry was presented which reveals that this joint replacement is performing better than the average. There have been a number of presentations which suggest that this knee replacement is associated with less anterior knee pain (pain at the front of the knee) and better stability whilst descending stairs than its predecessor. Clearly the long-term outcome of this knee replacement remains as yet unknown; however the results to date are very positive.
Following knee replacement you will usually be in hospital for 2 or 3 days depending on how well you can mobilise. In order to be safe to be discharged home you will be seen by the physiotherapists on a regular basis who will encourage you to move the knee as much as possible and provide you with exercises to practice. You will be provided with an ice pack to reduce swelling and help pain which you should use both in hospital and following discharge as much as possible. Once the physiotherapists are happy with your progress and you are safe on stairs, provided there are no medical problems Simon will be happy for you to be discharged home.
In order to reduce the risk of deep vein thrombosis you will have been given injections into the abdomen whilst in hospital. It is imperative that these are continue for 2 weeks following your surgery )unless alternative arrangements have been agreed with Simon) to minimise the risk of deep vein thrombosis. This is a serious condition and can occasionally result in pulmonary embolism. Following joint replacement surgery you should not fly for 6 weeks and should avoid a long-haul flight for 3 months because of the increased risk of deep vein thrombosis
When you are discharged home if needed you will be provided with a certificate signing you off work for 6 weeks. You will be signed off work for 6 weeks.
In terms of returning to driving you should take 6 weeks off driving unless your left knee has been replaced and you drive an automatic.
Arrangements will be made for you to be followed up by the physiotherapists but nevertheless please remeber it is really important that you continue to do the exercises you were shown in hospital at home.
You should take regular painkillers as needed – usually a combination of Ibuprofen and Paracetamol with codeine is sufficient.
You will be given an appointment for your clips to be removed 2 weeks following your surgery. You will also be given an appointment to be seen by Simon about 6 weeks following surgery when he will reassess your knee and discuss return to work and driving.
If needed Simon will then arrange to see you again at the 3-month post-operative stage. It takes approximately a year to reach an endpoint in recovery following joint replacement.
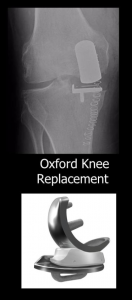 The treatment for knee arthritis depends on the severity of your symptoms. Sometimes arthritis may affect only part of your knee joint; for example if the arthritis affects only the medial compartment of the joint, as shown on this xray, a partial knee replacement to replace just the medial half of the joint can be the appropriate choice.
The treatment for knee arthritis depends on the severity of your symptoms. Sometimes arthritis may affect only part of your knee joint; for example if the arthritis affects only the medial compartment of the joint, as shown on this xray, a partial knee replacement to replace just the medial half of the joint can be the appropriate choice.
Simon uses the Oxford partial knee replacement produced by Zimmer Biomet which has an excellent track history. This partial knee replacement is inserted without bone cement and gradually bonds to your native bone.
Details of this partial knee replacement can be found here and consent information about partial knee replacement can be found here.
An Oxford partial knee replacement is usually carried out under a spinal anaesthetic. At the time of surgery final checks are made on the condition of the remainder of the joint to ensure that your knee is appropriate to receive an Oxford partial replacement. In general the post-operative recovery following a partial knee replacement is more rapid than a total knee replacement with many patients being discharged home on the first day following surgery.
Following your surgery you will have an x-ray to check the position of the prosthesis and will be mobilised by the physiotherapists progressing rapidly to crutches. It is important to move the knee as much as possible and to practice the exercises provided. An ice pack will be provided to reduce swelling and assist with pain control. You will also be provided with regular painkillers which are important for you to take.
As with all knee surgery, there is a risk of deep vein thrombosis and you will be given injections into the abdomen whilst in hospital. These need to continue for 2 weeks following your surgery unless alternative treatment has been discussed.
In addition to regular injection treatment you will also be provided with anti-embolism stockings which are to be worn for 6 weeks. Because of the increased risk of venous thrombo-embolism you should avoid flying for 6 weeks and long haul flights for 3 months.
When you are discharged home you will be provided with a certificate signing you off work for 6 weeks if needed and you should also plan to take 6 weeks off driving unless surgery has been carried out to your left knee and you drive an automatic.
Arrangements will be made for you to be followed up by the physiotherapists, but nevertheless please remember it is really important that you continue to do the exercises you are shown in hospital once you get home. You should also continue with regular painkillers as needed - usually a combination of ibuprofen and paracetamol with codeine is sufficient.
Your wound will be closed with clips and arrangements will be made for these to be removed 2 weeks following your surgery. You will also be given an appointment to be seen by Simon about 6 weeks following surgery when he will reassess your knee and discuss the need for ongoing physiotherapy, your return to work and to driving. If needed Simon will then arrange to see you again at the three-month post- operative stage.
It can take approximately a year to reach an endpoint in recovery following any type of joint replacement.
 Following dislocation of the patella generally treatment is conservative to strengthen the muscles which then maintains patella stability. Sometimes however physiotherapy treatment alone is insufficient to maintain patella stability long-term. In that case some form of patella stabilisation becomes necessary.
Following dislocation of the patella generally treatment is conservative to strengthen the muscles which then maintains patella stability. Sometimes however physiotherapy treatment alone is insufficient to maintain patella stability long-term. In that case some form of patella stabilisation becomes necessary.
The exact procedure required depends on a number of factors as described within the patella dislocation section of conditions treated. Surgery falls into either soft tissue stabilisation or bony stabilisation.
Bony stabilisation is required when there is altered alignment of the patellofemoral joint due to the position generally of the attachment of the patella tendon. The position of the patella tendon in relation to the groove in relation to the groove in which the patella sits in the femur determines whether a soft tissue procedure or a bony procedure is required.
In the case of a bony procedure generally this involves moving the attachment of the patella tendon to the tibia and then securing the attachment in the new position.
In the case of a soft tissue problem, this usually involves damage to the sheets of tissue adjacent to the medial border of the patella. This is known as the medial patella retinaculum and contains a ligament call the medial patellofemoral ligament.
Recently we have started to appreciate the damage to this ligament can result in patellar instability and with modern surgical techniques this ligament can be reconstructed using a hamstring tendon to provide a graft. This procedure is known as medial patellofemoral ligament reconstruction.
In general terms this is carried out using an arthroscopy of the knee to ensure that the patella will track normally and then harvesting a hamstring tendon through a small incision below the knee and threading it between the attachment of the medial collateral ligament to the femur and through the patella to make a new ligament which will restore stability.
You will have 3 small cut around the knee in addition to arthroscopy incisions. Following surgery which is generally carried out as a day case you will be mobilised with the help of physiotherapy but it is usual to have difficulty bending the knee to start with because the knee feels tight.
Following surgery most patients require at least a week off driving and 2 weeks off work and are unable to bend the knee comfortably for at least 6 weeks following the operation.
With intensive physiotherapy however the range of movement is gradually restored and this should be associated with a feeling of stability in the joint. It takes nearly a year to reach an endpoint in recovery but in terms of returning to sport, you can start this after about 6 weeks after surgery but should avoid twisting sport for a total of 3 months.
 Making the decision to go forward with revision knee surgery is always difficult as the risks and benefits of further surgery are less clear than undertaking a knee replacement for the 1st time.
Making the decision to go forward with revision knee surgery is always difficult as the risks and benefits of further surgery are less clear than undertaking a knee replacement for the 1st time.
The most important part of this decision-making process occurs in the outpatient setting when Simon explains the differing treatment options in your case.
Once the decision has been made to go forward with revision knee replacement, this may be carried out as a single operation when the initial knee replacement is removed and immediately replaced with a new knee replacement.
Revision knee replacement surgery is far more complex than the initial knee replacement surgery and often requires the use of special implants to support the new knee replacement safely within the bone.
In the case of infection revision knee surgery may be carried out as a two-stage procedure with initial removal of the knee replacement and insertion of temporary spaces which then requires a 2nd operation at a later date to remove the temporary spacers and insert a new knee replacement.
Between the stages of your revision knee replacement you will require antibiotic treatment to eradicate infection which requires a close liaison with a consultant microbiologist who will give advice about the correct antibiotic treatment for you.
Sometimes this will require a further procedure to insert a semipermanent intravenous line through which intravenous antibiotics can be given regularly.
The early recovery following revision knee replacement is generally slower than 1st time round however even in the case of a two-stage revision knee replacement you should be able to mobilise with crutches putting weight through the temporary replacement between the 2 stages.
As with a primary knee replacement procedure, it is imperative that you follow the physiotherapy exercises to maximise your recovery.
